Communication across generational lines always comes with challenges. For clued-up millennials and Gen Xers, cannabis has become a part of the cultural and therapeutic landscape. For many baby boomers, however, cannabis use is marred by stigma. It’s not exactly surprising–cannabis has (unjustly) had a bad rap for a long time.
In the early 20th century, cannabis became the target of a racially-charged smear campaign. Anti-cannabis propaganda saw cannabis heavily restricted under the 1937 Marihuana Tax Act, before being made federally illegal with the passage of the 1970 Controlled Substances Act. The stereotyping of cannabis users as stoners, and films such as Reefer Madness, helped further embed the idea that cannabis was used by deviants. The past few decades have seen public opinion about cannabis shift–but many still view cannabis in a negative light. 1 2
So, how do you go about explaining your cannabis use to a baby boomer–especially if they are your parent? Having open conversations about cannabis can undo decades of misunderstandings and misinformation, and may even help them understand that cannabis holds diverse therapeutic benefits.
Here are some important points you can tell them:
Cannabis rarely leads to harder substance use
What your parents may assume:
An accusation that’s often leveled at cannabis users is that cannabis is addictive.
What they need to know:
The existing scientific evidence about cannabis addiction is not so cut and dry. A comprehensive 2015 review of more than two decades of research found that individuals who try cannabis are less likely to develop a dependency than users of almost any other substance, including nicotine, heroin, cocaine, alcohol or stimulants. 3
The authors of the paper reported that the life-time risk of developing a dependence on cannabis was estimated at 9%. In contrast, the likelihood of developing a dependence on nicotine was a whopping 32%. Heroin came in at 23%, cocaine was 17%, alcohol was 15%, and stimulants were 11%. According to this study, more than nine out of every ten people who try cannabis do not become addicted and never will.
It’s also vital to recognize that although certain cannabinoids in cannabis can be addictive, others are not. Delta-9-THC increases the release of dopamine and opioid peptides, which can reinforce addictive behavior. Cannabidiol (CBD), on the other hand, has been shown the potential to treat addictive behaviors. A 2015 review found that CBD may be beneficial in treating opioid, cocaine, psychostimulant, cannabis and tobacco addiction. 45
Concerned parents also often worry that cannabis use paves the way for harder drug use, like cocaine, heroin, or methamphetamine; framing cannabis as a gateway drug. The vast majority of people who use cannabis, however, do not continue climbing a ladder towards harder drug use. Research instead suggests that rather than a generic ‘gateway effect’, cannabis affects users distinctly. 6 7 8
The National Institute on Drug Abuse (NIDA) emphasizes that a person’s social environment and personal circumstances represent a critical factor in a person’s risk for harder drug use.
Certain cannabis users appear more vulnerable to ‘the gateway drug effect’ than other cannabis users. The more vulnerable group tend to consume substances at a younger age and have more childhood problems with police, parents, friends, and school. Even according to NIDA, this gateway effect is not specific to cannabis, but rather to any substance use in adolescence including nicotine and alcohol. The authors pointed out that several factors may underpin this vulnerability, such as childhood trauma or negative peer influence.
Cannabis is less harmful than alcohol and tobacco
What your parents may assume:
Smoking cannabis is just as bad, if not worse, than drinking alcohol or smoking cigarettes
What they need to know:
Cannabis is significantly less harmful than either of these commonly used substances. Robust evidence indicates that cannabis is among the safest substances to use recreationally, with health risk exceedingly lower than alcohol, which should help to reassure a concerned parent. 9
Cannabis is approximately 114 times less deadly than alcohol, according to findings published in the journal Scientific Reports. The researchers carried out a risk assessment of seven drugs, with alcohol emerging as the riskiest, followed by heroin, cocaine, tobacco, ecstasy, methamphetamines, and cannabis taking last place. The mortality risk associated with each drug was calculated by comparing a lethal dose of each substance with the amount typically used. Not only was marijuana was the safest drug tested, but it was also classified as the only substance to have a low risk of mortality (both alcohol and tobacco were both found to have a high risk of mortality.) That’s not to say that marijuana can’t cause problems or harm–but when it’s weighed up against other substances, even those that are considered socially acceptable, it’s significantly less risky. 10
In a 2013 book, Marijuana is Safer: So Why Are We Driving People to Drink? the authors compared the safety record of cannabis with that of alcohol. The findings are clear–cannabis is also safer than alcohol from a social perspective. Alcohol is a major contributing factor to violent crime, including domestic abuse, sexual assault, and homicide. Cannabis on the other hand, is largely absent from such violent incidents. There’s also evidence that drivers under the influence of cannabis are significantly less likely to contribute to fatalities than those driving under the influence of alcohol. 11 12
Regular, heavy alcohol use can also lead to long-term brain damage. Cumulative cannabis use in adults, on the other hand, has not been linked to major changes in cognitive function. A study that tracked young adults until mid-adulthood found that cumulative lifetime exposure to marijuana was associated with lower scores on a test of verbal memory, but did not affect other cognitive abilities such as processing speed or executive function (executive function includes self-regulatory behaviors). However, THC use during adolescence may lead to problems with learning and memory later in life. 13 14 15
Cannabis can also claim a significant advantage over tobacco. Cigarette smokers inhale tar, carbon monoxide, ammonia are other harmful residues every time they light up and inhale. These contaminants can contribute to diverse forms of cancer, heart disease, stroke, lung diseases, diabetes, and chronic obstructive pulmonary disease (COPD). These tars and chemicals are also in the smoke of cannabis, but cannabis use is typically exceedingly less material per day compared to cigarettes. For example a 20 cigarettes per day smoker is considered normal, but that many joints in one day would be quite abnormal. Additionally, those who choose to ingest cannabis by vaping, applying topicals, or eating edibles, can sidestep the harms associated with smoking.
Finally, there’s currently no evidence that anyone has ever died from a cannabis overdose, whereas according to the CDC, alcohol poisoning kills six people every day in the United States. Even moreso, deaths related to excessive alcohol use are predicted to be around 260 deaths every day in the US alone.
Scientists are still unclear about what constitutes a lethal dose of THC in humans, but the dose that kills animals ranges from 40 mg/kg to 130 mg/kg (delivered intravenously). If the cannabis or THC is given orally, scientists have not yet identified the toxic dose in primates or higher mammals. A single joint can contain an average of 60 to 150 mg of THC–but not all the THC in the joint will be absorbed into the bloodstream. In other words, a cannabis user would need to smoke an extreme number of joints to even get close to a lethal dose. 16
Re-educating your parents about facts

After you’ve convinced your parents that cannabis use is actually less harmful than many other substances, it’s time to re-educate them on what cannabis is and can do.
Those who are unfamiliar with cannabis often associate it with THC and its psychoactive effects. There’s so much more to cannabis, however, than smoking and getting high.
Many cannabis skeptics are often surprised to learn that cannabis can represent an effective medicine for diverse conditions and disorders. Cannabinoids present in cannabis interact with the endocannabinoid system, which exists all throughout the body. This system functions as a fine tuning regulatory system for a large number of bodily functions, and therefore can be a useful therapeutic for many conditions.
Research into the diverse therapeutic applications of cannabis, and distinct cannabinoids is exploding. There’s already data that suggests cannabis may be effective in treating ailments as diverse as inflammation, pain, colitis, sleep disorders, neurological disorders, psychiatric disorders, and loss of appetite. Your parents may even find that cannabis could help with conditions that affect them. For example, non-psychoactive cannabidiol (CBD) has shown promise to ease pain and inflammation associated with arthritis. 17 18
Once you’ve piqued your parents’ interest, the next step is to walk them through the major cannabinoids, types of cannabis, and consumption methods. Getting back to basics can help the canna-cautious understand the plant from a more scientific perspective.
Here’s some entry-level information that’s perfect for sharing with cannabis beginners:
THC
THC is an abbreviation for delta-9 tetrahydrocannabinol, one of the major cannabinoids found in cannabis. THC is largely responsible for the intoxicating properties of cannabis, or the “high” that people experience. However, THC is also associated with many of the therapeutic effects associated with cannabis too.
THC possesses analgesic, antiemetic, anti-inflammatory, antioxidant, and neuroprotective properties, to name just a few of its characteristics. Even the FDA has approved the use of THC (in an FDA approved, lab-made form called Marinol©) for treating HIV/AIDS wasting syndrome and also nausea caused by chemotherapy.
When it comes to herbal-based cannabis, users who prefer cannabis strains with high concentrations of THC generally opt for delivery methods like smoking, vaping, edibles, or tinctures. The experience of THC can create feelings of euphoria or relaxation, but also anxiety and paranoia (these negative effects are often associated with higher doses). 19
CBD
Cannabidiol, or CBD, is another major cannabinoid found in cannabis. Unlike THC, CBD is non-intoxicating, although it still has psychoactive properties (which means it can cause changes in mood, awareness, feelings, or behavior). CBD has also been linked to diverse therapeutic properties: it’s anticonvulsive, antioxidant, antipsychotic, analgesic, and antiinflammatory. Users who take CBD often note that it leaves them feeling calm, relaxed, and at ease–but not everyone reports the same experience. The most common methods for consuming CBD are in a tincture format, as edibles, or as a topical. There is also cannabis flower which is low in THC but high in CBD, known as hemp flower or Type III cannabis.
Types of cannabis
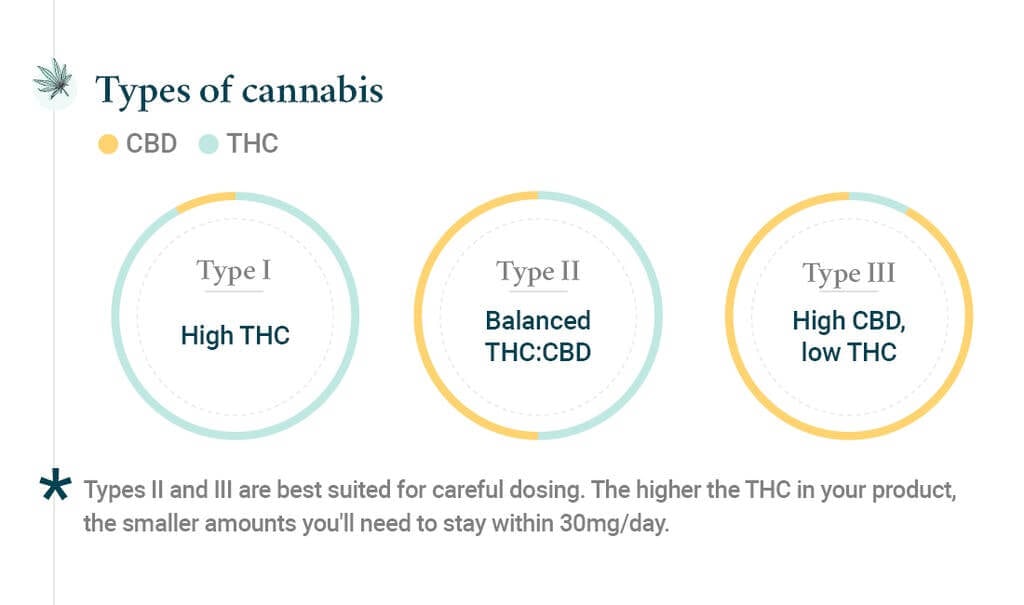
Cannabis can be categorized into three groups, with each group or “chemotype” defined by its most abundant cannabinoid.
- Type I cannabis is THC dominant. There are more than 100 cannabinoids that can be present in cannabis, but in Type I cannabis, THC is the most prolific.
- Type II cannabis has a balanced ratio of CBD and THC as the dominant cannabinoids, with other minor cannabinoids playing the supporting role.
- Type III cannabis has a high ratio of CBD, with trace amounts of THC and other cannabinoids. There are more chemotypes (ex Type IV) that have been proposed, but at this time there is no scientific consensus on their definition.
People who use cannabis for recreational reasons will tend to opt for Type I, as it is the best known and also the most widely available. Medical patients are often started on a Type II product as general consensus among cannabis clinicians is that this balance works best for most patients. People who are looking to get the benefits of cannabis but avoid the intoxication are more likely to lean towards CBD-dominant, Type III strains.
Consumption methods
Old-school consumption methods such as bongs, pipes, and joints are partly responsible for the stigma that has stuck to cannabis for so long. Nowadays, however, there’s a diversity of sophisticated, easy-to-use products that enable cannabis consumption without smoking. Teaching your parents about the diverse ways you can ingest cannabis will help them realize that cannabis isn’t just for pot smokers–it’s for people looking to ease pain with a topical cream, or ease anxiety with a drop of tincture under their tongue.
Consumption methods, or delivery methods, can broadly be separated into three groups based on the way they are taken into the body: inhalation, oral consumption, and topicals. Within these broader categories, there are also subcategories–in short, there’s a delivery method to suit every preference and purpose. Each delivery method is associated with its own onset time (the time it takes to start working) and duration of effects.
- Inhalation methods include smoking, pipes, bongs, dry herb vaporizers, vape pens (which use an oil cartridge), dab rigs and aerosolized metered dose inhalers.
- Oral consumption methods include edibles, tinctures, oils, sprays, and capsules. Some of these are sublingual, meaning they may be more rapidly absorbed into the bloodstream, while others are processed through the digestive system and liver (which takes longer).
- Topicals are designed for external application and include creams, balms, oils, transdermal patches, salves and serums. Some topicals permeate the skin for localized relief, while others may be able to permeate through the skin into the bloodstream, providing more whole-body relief.
Let the science speak for itself
If your parents are concerned about your cannabis use, the most effective way to allay their fears is with scientifically sound facts. Biased ideas about cannabis are often rooted in misinformation and decades old propaganda.
Certain generations, such as the baby boomers, grew up in a time where cannabis use was saturated with stigmatization. By deconstructing beliefs about addiction, emphasizing the relative safety of cannabis compared with other common substances, and educating your parents about the benefits and uses of cannabis, you’ll help them set aside their preconceived notions.
Who knows, they may even become curious about trying cannabis for themselves.
Sources
- Robert Solomon.Cannabis and Cannabinoid Research.Mar 2020.2-5.http://doi.org/10.1089/can.2019.0063
- Musto DF. The Marihuana Tax Act of 1937. Arch Gen Psychiatry. 1972;26(2):101–108. doi:10.1001/archpsyc.1972.01750200005002
- Hall W. (2015). What has research over the past two decades revealed about the adverse health effects of recreational cannabis use?. Addiction (Abingdon, England), 110(1), 19–35. https://doi.org/10.1111/add.12703
- Curran, H., Freeman, T., Mokrysz, C. et al. Keep off the grass? Cannabis, cognition and addiction. Nat Rev Neurosci 17, 293–306 (2016). https://doi.org/10.1038/nrn.2016.28
- Prud’homme, M., Cata, R., & Jutras-Aswad, D. (2015). Cannabidiol as an Intervention for Addictive Behaviors: A Systematic Review of the Evidence. Substance Abuse: Research and Treatment. https://doi.org/10.4137/SART.S25081
- NIDA. (n.d.) Is cannabis a gateway drug? Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/marijuana-gateway-drug
- Melberg, H. O., Jones, A. M., & Bretteville-Jensen, A. L. (2010). Is cannabis a gateway to hard drugs?. Empirical Economics, 38(3), 583-603.
- NIDA. 2021, May 24. Is marijuana a gateway drug?. Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/marijuana-gateway-drug on 2021, November 28
- Hall W. (2015). What has research over the past two decades revealed about the adverse health effects of recreational cannabis use?. Addiction (Abingdon, England), 110(1), 19–35. https://doi.org/10.1111/add.12703
- Lachenmeier DW, Rehm J. Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach. Sci Rep. 2015;5:8126. Published 2015 Jan 30. doi:10.1038/srep08126
- Fox, S., Armentano, P., & Tvert, M. (2013). Marijuana is safer: so why are we driving people to drink?. Chelsea Green Publishing.
- Lachenmeier DW, Rehm J. Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach. Sci Rep. 2015;5:8126. Published 2015 Jan 30. doi:10.1038/srep08126
- Sullivan EV, Harris RA, Pfefferbaum A. Alcohol’s effects on brain and behavior. Alcohol Res Health. 2010;33(1-2):127-143.
- NIDA. 2021, April 13. What are marijuana’s long-term effects on the brain?. Retrieved from https://www.drugabuse.gov/publications/research-reports/marijuana/what-are-marijuanas-long-term-effects-brain on 2021, November 28
- Auer, R., Vittinghoff, E., Yaffe, K., Künzi, A., Kertesz, S. G., Levine, D. A., Albanese, E., Whitmer, R. A., Jacobs, D. R., Jr, Sidney, S., Glymour, M. M., & Pletcher, M. J. (2016). Association Between Lifetime Marijuana Use and Cognitive Function in Middle Age: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA internal medicine, 176(3), 352–361. https://doi.org/10.1001/jamainternmed.2015.7841
- Turner AR, Spurling BC, Agrawal S. Marijuana Toxicity. [Updated 2021 Aug 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430823/
- Bonini, S. A., Premoli, M., Tambaro, S., Kumar, A., Maccarinelli, G., Memo, M., & Mastinu, A. (2018). Cannabis sativa: A comprehensive ethnopharmacological review of a medicinal plant with a long history. Journal of ethnopharmacology, 227, 300-315.
- Hammell DC, Zhang LP, Ma F, et al. Transdermal cannabidiol reduces inflammation and pain-related behaviours in a rat model of arthritis. Eur J Pain. 2016;20(6):936-948. doi:10.1002/ejp.818
- Crippa, J. A., Zuardi, A. W., Martín‐Santos, R., Bhattacharyya, S., Atakan, Z., McGuire, P., & Fusar‐Poli, P. (2009). Cannabis and anxiety: a critical review of the evidence. Human Psychopharmacology: Clinical and Experimental, 24(7), 515-523.
Sign up for bi-weekly updates, packed full of cannabis education, recipes, and tips. Your inbox will love it.

 Shop
Shop Support
Support


















